From Bump to Baby and Beyond:
Your Complete Prenatal Care Kit
Bookmark this page to refer back to later.
From Bump to Baby and Beyond: Your Complete Prenatal Care Kit
Practical Considerations for Your Pregnancy
During your pregnancy, the best thing you can do for yourself and your baby is to take care of your health. You’ll be experiencing significant physical changes over the next nine months, so be patient with your body. It’s important to care for your emotional health too, especially since many women also experience more frequent mood swings during pregnancy. Although every pregnancy is different, here are a few recommendations to guide you.
Diet & Exercise
During your pregnancy, you’re eating for two. This doesn’t mean you need to double the calories, though. In fact, in the first trimester, you will not need a large increase in your calorie intake. By the second trimester, you’ll require an additional 340 calories per day and during the third trimester, you’ll need to consume an additional 450 calories.
It’s also a good idea to take a prenatal vitamin to cover any gaps in your nutrition. Most women choose a prenatal vitamin with iron levels that meet their daily requirement. For more nutrition information, visit ChooseMyPlate.org.
Food Safety
During your pregnancy, you may experience a heightened sense of taste, and your food preferences may change. Listen to your body’s changing wants and needs. You’ll also want to keep the following food safety recommendations in mind.
During your pregnancy, you should avoid the following foods:
- Seafood high in mercury (more information)
- Raw or undercooked seafood
- Undercooked meat, poultry and eggs
- Under-pasteurized foods
- Unwashed fruits or vegetables
Listeria is a serious infection usually caused by eating contaminated food. Listeria affects 1/8000 pregnancies a year and can lead to miscarriage, preterm birth and stillbirth. Surviving infants are likely to be born prematurely and may suffer serious infections and/ or neurological problems.
Reduce your risk of contracting listeria by avoiding foods that have been in you refrigerator beyond their expiration date and by washing all fruits and vegetables. Although most outbreaks are sporadic, raw-milk cheeses and deli meats are two higher-risk foods.
The risk of congenital toxoplasmosis can be reduced by 50% by avoiding raw/ rare meat and poultry and by washing all fruit and vegetables. Cats are NOT a common source of toxoplasmosis. Long time cat owners have likely been exposed and thus their pregnancies are not at risk. Use caution when handling young kittens as they may pose more of a risk.
For more information on food safety visit: www.FDA.gov.
Keep in mind that no amount of nicotine, alcohol or illicit drugs are considered safe during pregnancy. Using these substances is a direct cause of complications including Fetal Alcohol Syndrome, stunted growth, preterm delivery, and placental abruption (where the placenta separates from the uterine lining). If you need help staying sober, or are currently in a treatment program, don’t be ashamed - reach out to your health provider. They will work with you to ensure a safe and healthy pregnancy.
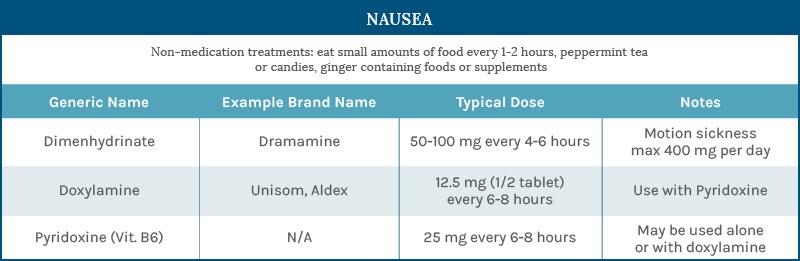
Nausea
Nausea in pregnancy is known as morning sickness, but frequently occurs at other times of the day or evening. It is usually worse in the morning since the stomach is empty.
The cause of nausea and pregnancy is not known, although the rapidly rising hormone levels in early pregnancy are believed to be a factor. Fortunately, it usually only occurs during the first three months of pregnancy.
Megan Bina, D.O.
OBSTETRICS & GYNECOLOGY
Reducing nausea: There are numerous techniques to reduce nausea. Not all of them work for all women. Try any one, or all, or any combination, until you find what works best for you.
Remember: If you go 24 hours without retaining any food or liquid, you should contact your doctor immediately. If nausea, with or without vomiting, is interfering with your daily life, and the below measures are not helping, please call your doctor.
- Don't let your stomach get completely empty. This is a vicious cycle: you are not hungry because you are nauseated, but if you go too long without eating, the nausea can get worse. Small meals are tolerated better than larger ones. Plan out what you need to eat for the day to meet your minimum nutritional requirements. Eat a few bites every hour or two and space your total amount of fluids our over the day. If you need to use the bathroom during the night, take a few minutes to each a small bite of food.
- Keep some crackers, dry toast, popcorn, or other dry carbohydrate food at your bedside and eat a little of it before you get out of bed in the morning.
- Eat or drink something sweet (like fruit or fruit juice) before going to bed at night and before getting up in the morning.
- Avoid spicy foods and foods with strong or offensive odors.
- Avoid fats in your diet. These can be especially nauseating.
Some women discover a certain food that just doesn't agree with them during pregnancy. If you get extremely nauseated after eating any particular food 2 or 3 times in a row, you may have to give it up for the duration of your pregnancy.
Jacinda Serberio, M.D.
OBSTETRICS & GYNECOLOGY
- Suck on lemon drops, hard candy, or life savers throughout the day.
- Drink peppermint tea, which can settle the stomach and relieve nausea.
- Take vitamin B6, which can help relieve nausea if taken in large doses. Most prenatal vitamins only contain about 5 mg, so you’ll want to purchase vitamin B6 by itself and take 25 mg 3 times a day.
- Take Unisom with your vitamin B6. Unisom is an over-the-counter sleeping pill which decreases morning sickness symptoms when taken with vitamin B6. The usual dosage is one Unisom tablet taken with 25 mg of vitamin B6, once in the morning and once at bedtime. Since sleepiness can be a side effect, you may want to try half a Unisom tablet in the morning. The combination of Unisom and vitamin B6 is safe during pregnancy.
Weight Gain
Exercise
Exercise has many benefits during pregnancy. Regular exercise can reduce or prevent back pain, prevent excessive weight gain, and reduce the risk of gestational diabetes and high blood pressure.
Thirty minutes of moderate exercise on most or all days of the week is recommended for women without obstetrical or medical complications. “Moderate” exercise means that you should be able to carry on a normal conversation.
Leslee Jaeger, M.D.
OBSTETRICS & GYNECOLOGY
During pregnancy, you should avoid activities with a high risk of falling or abdominal trauma, exercise at high altitudes and scuba diving. If you have questions about specific activities please ask your provider.
General Care & Advice
Dental Care
It can be tempting to put off other types of medical appointments during your pregnancy. However, it’s important to see your dentist regularly and not to put off routine care or other dental treatments.
Sherry Paulson, M.D.
Hormonal changes during pregnancy can make you more susceptible to periodontal disease and gingivitis (tender gums). Keep your regularly scheduled appointments to reduce your risk of contracting these diseases.
OBSTETRICS & GYNECOLOGY
Routine dental care and treatment of dental conditions should not be delayed or avoided because of pregnancy. Dental x-rays (with proper shielding) and procedures such as tooth extraction, cavity filling, etc. are not harmful to your pregnancy. If you have questions or concerns about a specific dental procedure please let your provider know.
Baths
It’s fine to take baths during your pregnancy as long as the water isn’t too hot. However, you should avoid hot tubs and saunas during your first trimester.
Sexual Activity
In most cases, pregnant women can continue sexual intercourse. However, intercourse should be suspended if you experience specific pregnancy complications like preterm labor, unexplained vaginal bleeding, leaking amniotic fluid, premature cervical dilation, placenta previa, or vasa previa.
Work
Although you may need certain adjustments to your work style, in general, women can plan to work throughout a pregnancy.
To stay comfortable at work, take short frequent breaks, use a chair with good lower back support, wear flat shoes with good support and consider wearing support stockings.
Sarah Tillman, M.D.
OBSTETRICS & GYNECOLOGY
Driving
Everyone should wear a seatbelt when traveling by car. Although many pregnant women find seatbelts restricting or uncomfortable, they should be worn 100% of the time during pregnancy. Increase effectiveness and comfort by placing the lap belt across the hips and below the abdomen, and the shoulder belt between the breast and to the side of the abdomen.
Do NOT turn airbags off – they are designed to provide cushioning and protect against more serious injuries in case of a crash.
Flying
Most airlines allow travel up to 37 weeks gestation; however, individual carriers may have different policies. Commercial airlines travel is generally safe for those with uncomplicated pregnancies.
If you fly during your pregnancy, use these tips to stay comfortable and safe:
• Get out of your seat and walk every 1-2 hours to help prevent blood clots in your legs
• Consider wearing compression stockings, which can also help prevent blood clots
• Wear loose, non-restrictive clothing
• Discuss travel plans with your provider
• Travel with a copy of your prenatal records
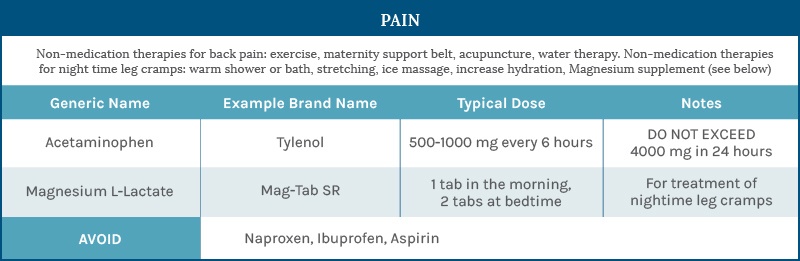
Medications & Pregnancy
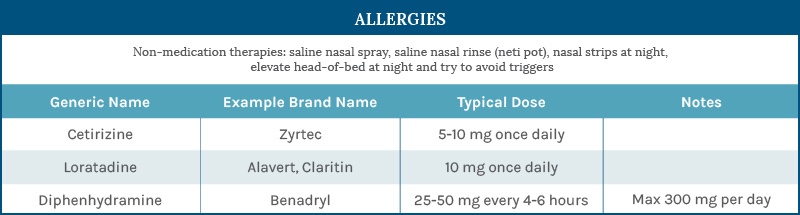
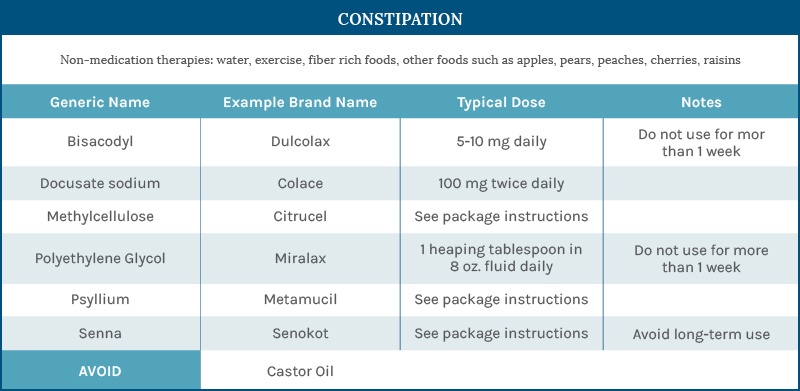
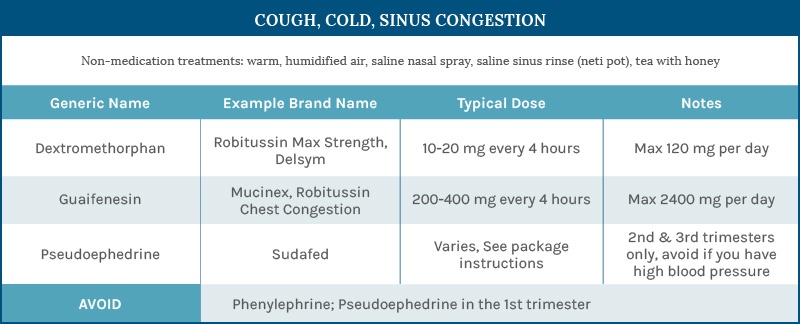
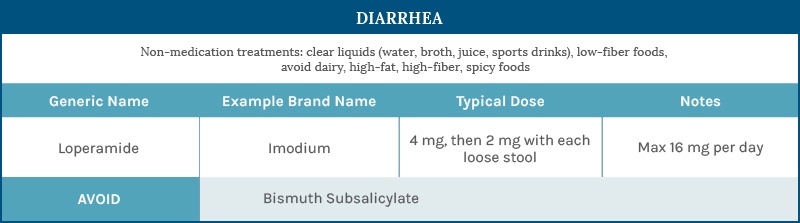
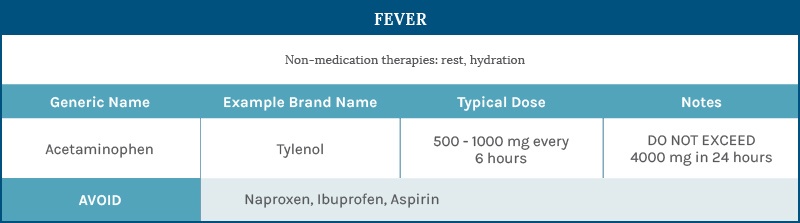
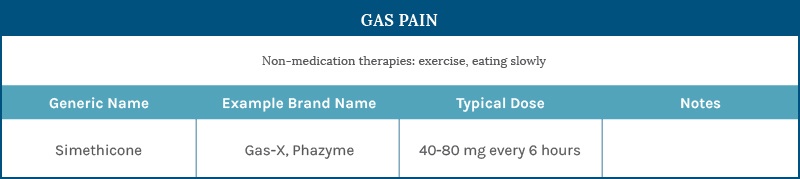
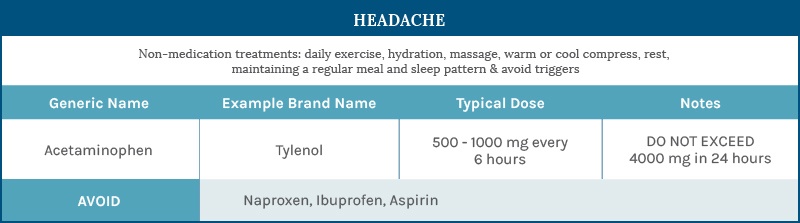
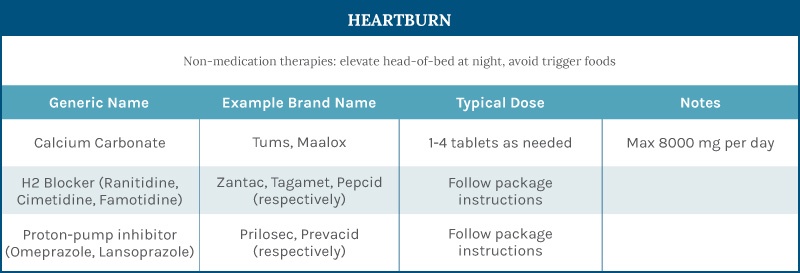
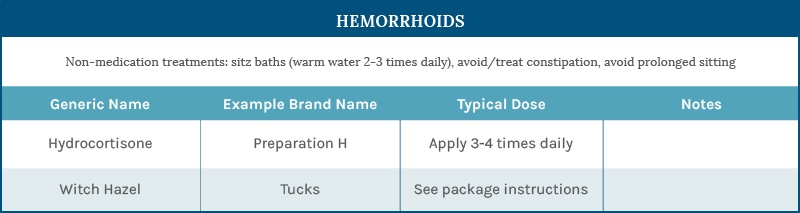
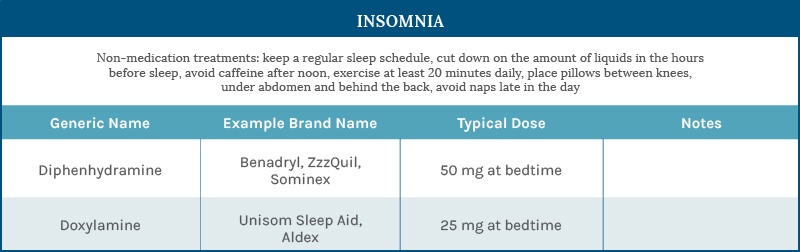
Few medications have been approved to be used during pregnancy. However, the medications listed below have not been shown to increase the risk of birth defects or adverse pregnancy outcomes when taken as directed.
Before you take any medication during pregnancy, it's important to weigh the severity of your symptoms against possible risks to your baby.
Karen Collins, APRN, CNP
OBSTETRICS & GYNECOLOGY
For more information, visit MotherToBaby.org or talk to your provider.
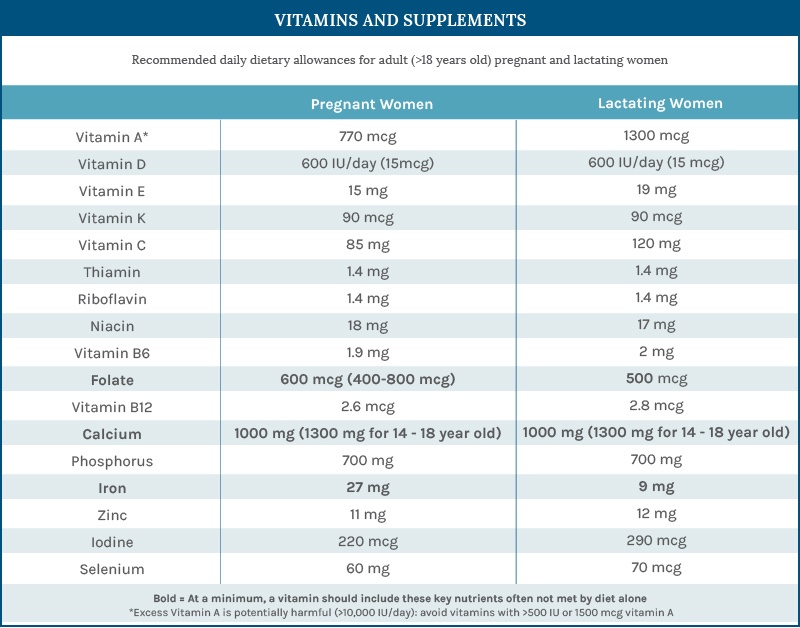
Vitamins & Supplements
Prenatal Vitamins
Though most well-nourished women meet nutrient needs by diet alone, it’s recommended that you take a prenatal vitamin if you are pregnant or planning to become pregnant.
Cristen Singer, APRN, CNP, CLC
OBSTETRICS & GYNECOLOGY
At a minimum, iron, folate and calcium should be supplemented (see below for dosing).
Herbal Medicines
The strength and purity of herbal medicines is unregulated. Herbal preparations can interact with commonly prescribed medications and lead to dangerous side effects. We recommend avoiding herbal supplements (with the exception of ginger for nausea).
How to Evaluate a Women’s Health Clinic [Checklist]
You’re expecting — congratulations! It’s going to be an extremely exciting nine months. One of the biggest decisions you’ll need to make (besides choosing your baby’s name) is which women’s health clinic you’re going to trust for all of your prenatal needs.
You’re expecting — congratulations! It’s going to be an extremely exciting nine months. One of the biggest decisions you’ll need to make (besides choosing your baby’s name) is which women’s health clinic you’re going to trust for all of your prenatal needs.
From the initial appointment, to the actual delivery, and all the check-ups in between, you’ll be seeing a lot of your prenatal provider. Different clinics have different approaches have different approaches to prenatal care, and it can be overwhelming to decide which clinic is the best option for you and your baby.
If you’re currently looking for a women’s health clinic, there are many factors you’ll want to consider. We’ve put together this checklist to help you evaluate potential clinics.

BEFORE YOUR APPOINTMENT
Before you visit a clinic for the first time, make sure it meets these requirements:
My insurance covers visits at this clinic
The option to see a female provider if I prefer
I can switch providers at any time during my pregnancy
The clinic’s website has clear, helpful information about services
It’s easy for me to schedule an appointment
I know what to expect at my first appointment, and what information to bring with me
DURING YOUR APPOINTMENT
While you’re at your first prenatal appointment, make sure the clinic meets the following requirements:
The clinic is conveniently located
Appointments are offered at times that meet my needs
Parking is easy to find
Facility is modern and up-to-date
Clinic uses state-of-the-art technology and equipment
Waiting rooms are clean, organized, and calming
Staff is welcoming, helpful, and attentive to my needs
Wait times are short and I am a priority for my doctor
My doctor listens to me and addresses my questions and concerns
I am introduced to any medical providers who may be a part of my care
I feel comfortable with my doctor and the clinic’s atmosphere
AFTER YOUR APPOINTMENT
Once you’ve arrived home, you should be able to confidently answer “yes” to the following:
I know when to schedule my next appointment
I feel comfortable with the length of time between appointments
I was given resources and information to help me care for my body and my baby
If I have questions or concerns, I know who to contact and the hours they’re available
Overall, I was satisfied with my experience at the clinic
It’s important that you feel comfortable with your prenatal care and confident that you’ve made the right decision for yourself and your baby. Check off these requirements to find the quality of care both of you need and deserve.
How to Make the Most of Your First Prenatal Visit
Your first prenatal visit usually takes place when you are about 8-10 weeks pregnant. This appointment is often the longest, and will include a general physical and routine prenatal labs.
After your first appointment, prenatal appointments typically last as little as 15 minutes for uncomplicated pregnancies. Make sure that your provider answers any questions you have at these appointments, but don’t worry if your appointment feels short - a quick appointment is usually a good sign that your pregnancy is progressing normally.
For an uncomplicated pregnancy, women should plan to see their provider every 4 weeks through 28 weeks, every 2 weeks between 28 and 36 weeks, and weekly from 36 weeks to delivery. Every visit will include a weight check, blood pressure check, and a chance to listen to the fetal heart beat.

Your first prenatal appointment is one of the most important visits. Your doctor will take your medical history, and help you form a plan for your prenatal care. This is also a great time to ask any questions you have.
Here are three steps to help you make the most of your first prenatal visit.

1. Gather important medical information before you go.
Before you arrive at your appointment, you’ll want to educate yourself about your medical history. This medical history is more extensive than ones taken at check-ups, so make sure you have knowledge (and documentation, when possible) of the following details.
Your partner’s medical history will also affect the health of your baby, so he should attend this appointment if possible. If you or your partner were adopted, or if you used a donor egg or sperm, you may have less genetic information available to you, but your doctor will help you interpret the information you do have.
Make sure to include:
- General Medical History: Include any medical problems you have or have had. List types, dates, and treatments if applicable. Your doctor may classify your pregnancy as high-risk if you suffer from health problems including diabetes, cancer, kidney disease, epilepsy, or high blood pressure.
- Family Medical History: Your baby may be at higher risk for certain genetic disorders if they run in your family or your partner’s family. Ask family members about genetic disorders and birth defect history. Depending on your family medical history, your ethnic background, and other factors, your provider may recommend different screenings or tests. For example, people of Ashkenazi Jewish heritage have an increased risk of Cystic Fibrosis and Tay-Sachs Disease, and people of African descent have an increased risk of sickle cell disease.
- Fertility History: List your menstrual history, including regular/ irregular periods, history of cramping or PMS, and any medication you use to bring on a period. Describe any fertility treatments you have had and their outcomes. Include your pap smear history, any abnormalities detected, and treatments if applicable (ie ie colposcopy, cryosurgery, laser treatment, conization, LEEP procedure).
- Past Pregnancies: Include live births, stillbirths, premature deliveries (less than 37 weeks), miscarriages (less than 20 weeks), ectopic/ tubal pregnancies, and/or elective terminations (abortions).
- Infection Exposure: Include chlamydia, gonorrhea, herpes, genital warts/ HPV, syphilis, HIV/AIDS, hepatitis.
- Medications You’re Taking: Include prescription as well as over-the-counter medications in this list. Also make a list of any herbal medicines, vitamins, or health supplements you take. Note any allergies to medication.
- Dietary Habits: Your doctor will ask about your caffeine, alcohol, and nicotine consumption. A moderate amount of coffee can be consumed during pregnancy, but no amount of nicotine, alcohol, or illicit drugs are considered safe. If you need help staying sober, reach out to your provider, and they will work with you to ensure a safe and healthy pregnancy.
- Mental Health History: Let your doctor know if you have a history of anxiety, depression, or other mental health conditions. Your doctor will help you find a treatment plan that cares for you and your baby. In some cases, your doctor may recommend that you stop taking a certain medication. However, in other cases, the risks of stopping a medication outweigh the potential benefits. Talk to your doctor to find the plan that’s right for you.
2. Know what to expect at your first prenatal appointment.
Your first prenatal visit is usually the longest unless you experience complications with your pregnancy.
Routine Procedures
At this appointment, your provider will take your medical history, check your weight and blood pressure, and perform blood tests. These blood tests will test your blood type, Rh factor, exposure to hepatitis and syphilis, and immunity to German measles.
Fetal Heartbeat
You may be able to hear your baby’s heartbeat at this appointment. However, if your prenatal appointment is on the earlierside, you may need to wait to hear your baby’s heartbeat. The fetal heartbeat is usually first detectable between 12 and 14 weeks.
HIV Testing
You may choose to take an HIV test during the early stages of your pregnancy. Any person who is sexually active is at least potentially at risk for HIV infection. Many people who are HIV positive do not belong to any particular high risk group, such as drug users.
HIV in pregnancy has potentially serious implications for mother and baby. We now have the capacity to offer medications in pregnancy to help prevent transmission of the virus to the baby. Obviously, we cannot offer medications unless we know your HIV status. Most women will have a normal or negative result and will be relieved by having this information. If you do test positive, we will help you in obtaining specialized care for both yourself and your baby.
Prenatal Care Plan
Finally, your provider will go over recommendations for your prenatal care, including diet, exercise, sexual activity, travel, and work. You’ll go over your appointment schedule for the course of your pregnancy, and should also go over a plan for your general health. You may be at the doctor more frequently than usual during your pregnancy, but it’s important not to put off other regular procedures, like your regular dental checkup.
3. Have a list of questions to ask your doctor.
Depending on your unique situation, you may have many different questions for your doctor. Here are our top 10 questions all women should ask at their first prenatal visit:
- Are there changes I should make to my diet? Throughout your pregnancy, try to consume a wide variety of foods, including lean meats, whole grains, fruits, vegetables and unsaturated fats. Many women also take prenatal vitamins. Talk to your doctor about specific dietary recommendations.
- What foods should I avoid during pregnancy? Pregnant women should avoid raw or undercooked seafood such as sushi. Avoid unwashed fruits or vegetables to reduce your risk of congenital toxoplasmosis. Your doctor will look at your diet and help you avoid other foods that may harm your baby.
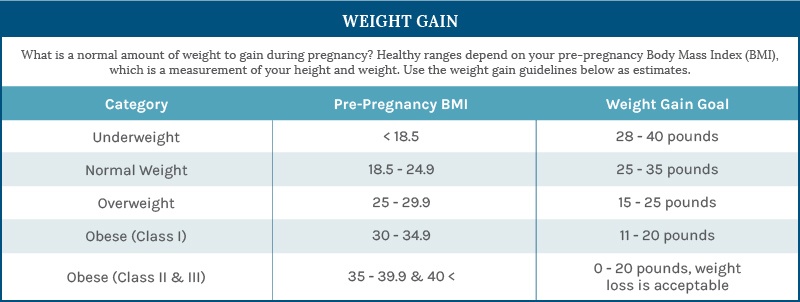
- How much weight should I expect to gain during my pregnancy? Healthy weight gain ranges depend on your pre-pregnancy BMI. Your doctor will help you establish healthy weight gain goals.
- How much should I be exercising? Regular exercise can reduce or prevent back pain, prevent excessive weight gain, and reduce the risk of gestational diabetes and high blood pressure. However, pregnant women should avoid activities with a high risk of falling or abdominal trauma, exercise at high altitudes, and scuba diving. Ask your doctor if you have questions about specific activities.
- Can I travel during my pregnancy? Many pregnant women drive throughout their pregnancies. Many women also fly until late in their pregnancies, and most airlines allow travel up to 37 weeks gestation. Talk to your doctor about safety measures to take when traveling.
- Will I be able to work throughout my pregnancy? Although you may need certain adjustments to your work style, in general, women can plan to work throughout a pregnancy. Talk to your doctor about strategies to stay comfortable at work, and what to do if you need special accommodations.
- Can I continue taking my current medications? Few medications have been approved to be used during pregnancy. However, certain medications have not been shown to increase the risk of birth defects or adverse pregnancy outcomes when taken as directed. Before you take any medication during pregnancy, it’s important to weigh the severity of your symptoms against the possible risks to your baby. Ask your doctor for more information about specific medications.
- When will my next appointment be? For an uncomplicated pregnancy, women should plan to see their provider every 4 weeks through 28 weeks, every 2 weeks between 28 and 36 weeks, and weekly from 36 weeks to delivery. Your doctor may wish to see you more frequently if you have a high-risk pregnancy. Talk to your doctor about a plan for your prenatal care during this first appointment.
- Do you recommend any type of prenatal screening or testing? Depending on factors like your family medical history and your ethnic background, your doctor may recommend prenatal screening or testing. The decision to pursue prenatal screening or testing is personal, and there is no one right path. Your doctor will help you make an informed decision that is right for you.
- Do you recommend any prenatal classes? To prepare for delivery, you may also want to take a prenatal class. There are many different options for delivery, so you’ll want to choose a class that fits your needs. Ask your doctor about finding the right class for you.
Use these recommendations to make the most of your first prenatal visit. And remember – don’t be afraid to reach out to your doctor with questions! Your health, and your baby’s health, is their priority.
What to Expect With Testing & Screening
Today, modern technology makes it possible to know more than ever before about your baby before he or she is born. In addition to routine prenatal appointments, you may wish to consider various types of prenatal testing. Below, you’ll find some common tests and their benefits. Different tests can be performed at different stages in your pregnancy, and they are listed in order below.
While there are no tests in pregnancy which provide a 100% guarantee of a normal outcome, chances are in your favor, even with an increased risk assessment, of having a healthy baby.

Carrier Screenings
A carrier screening is done on parents or prospective parents to see whether they carry an abnormal gene for a disorder which could be passed on to their child. A carrier has mild or no symptoms of a disorder, making testing important.
A carrier is someone with mild or no symptoms of a disorder but carries an abnormal gene for a disorder which can be passed on to their child. Carrier screening is performed through a blood test. If you are found to be a carrier, your partner is then screened for the disorder. If you are not a carrier, no additional testing is done.
Carrier screening can be done before or during pregnancy. People of certain ethnic groups are more likely to be carriers of different diseases; below you will find more information on the most commonly screened for disorders. All carrier screening has limitations; if you decide to pursue carrier screening you will meet with a genetic counselor to learn about these limitations. Results are usually available within 2-3 weeks.
If you and your partner are both carriers for the same disorder, you may wish to have your baby tested. Ask your healthcare provider or a genetic counselor about your options.
Since these screenings are performed on the parents or prospective parents, they do not need to be re-performed with a subsequent pregnancy.

Prenatal Screening: First Trimester
Non-invasive Prenatal Testing (NIPT)
Non-invasive prenatal testing (NIPT) is a screening test performed any time after 10 weeks 0 days and identifies women whose fetuses are at risk of having an abnormal number of chromosomes. Two of the most common are an extra chromosome (“trisomy”) or a missing chromosome (“monosomy”). There are three common trisomy conditions: trisomy 21 (Down Syndrome), trisomy 13 (Patau Syndrome), and trisomy 18 (Edwards Syndrome). A common monosomy is monosomy X (Turner Syndrome). The risk of having an abnormal chromosome count increases with a mother’s age.
First Trimester Screen (FTS)
The first trimester screen (FTS) is a prenatal test that is performed between 11 weeks + 6 days and 13 weeks + 6 days of pregnancy and screens for the risk of trisomy 13, 18, and 21. FTS combines two blood markers (PAPP-A and Beta-HGC) and an ultrasound measurement of the thickness of the back of the fetal neck (nuchal translucency). The FTS results provide a revised risk for trisomy 13 18, and 21 that may be higher or lower than the pre-screen, age-based risk. It does not diagnose the problem definitively.
Follow-up Testing
If you have an abnormal NIPT or FTS, you will be referred to a genetic counselor and offered diagnostic testing (such as amniocentesis). The decision to pursue diagnostic testing is a personal decision. The advantage of screening early in your pregnancy is obtaining earlier information about your pregnancy which may allow for more options regarding the pregnancy as well as more time to make those decisions. A genetic counselor will review what your options are for diagnostic testing.
If you opt for NIPT or FTS, you will be offered separate screening for neural tube defects in the second trimester.

Prenatal Testing: Second and Third Trimester
Anatomy Ultrasound: 20 weeks
Women usually have at least one ultrasound during their pregnancy. The first ultrasound is usually performed around 20 weeks.
Your baby will be screened for anatomical and placental abnormalities, and abnormalities that increase the risk for aneuploidy. You may also find out the sex of your baby if you wish. If this first "Level 1" ultrasound detects an abnormality, or you have a medical condition associated with increased risk for birth defects, a “Level 2” ultrasound can be used to tell you more about the possible risks. Remember that not all abnormalities can be detected by ultrasound. Diagnostic screenings and/ or tests will tell you more about your baby.
Gestational Diabetes and Anemia Screening: between 26 to 28 weeks
Gestational diabetes occurs when your body is not able to produce enough insulin during pregnancy. Many hormones secreted by the placenta are insulin inhibitors, so women who are not usually at risk of developing adult-onset (type 2) diabetes can still be affected by gestational diabetes.
If you develop gestational diabetes, diet and exercise changes may be enough to manage this disease. However, women will occasionally need to take insulin shots or diabetes medications to manage symptoms. When untreated, gestational diabetes can lead to high blood pressure and preeclampsia, larger babies, higher risk of c-section and increases your baby’s risk for neonatal (infant) diabetes.
Iron deficiency anemia is common during pregnancy because your body’s blood volume doubles and babies need a lot of oxygen. If you develop iron deficiency anemia, your doctor may recommend a multivitamin high in iron, or dietary changes to increase your consumption of meats like chicken, turkey, and beef; or other foods like beans, tofu, spinach, or brown rice.
Tetanus and Diphtheria (Whooping Cough) Vaccine: 28 weeks
The CDC recommends getting the Tdap vaccine between 27-26 weeks. This helps pass immunity to your baby. Getting the vaccine earlier within this timeframe may maximize its effectiveness for your baby. (See these CDC immunization guidelines for pregnant women for more details).
Rh0(D) prescription (for Rh negative blood types): 28 weeks
Rh is a protein found on the surface of red blood cells. About 85% of the population carries the Rh positive protein. If you are Rh negative, and your partner is Rh positive, there is a 50% chance that your baby will be Rh positive. When the baby is positive and the mother is negative the mother’s immune system can be triggered (sensitized) to attack the baby’s bold cells.
If you are Rh negative your doctor will prescribe an Rh immunoglobulin shot like RhoGAM. This will prevent Rh sensitization.
Rh sensitization may not affect the first pregnancy as severely, however, if you become pregnant with another Rh-positive fetus, the reaction will be severe and even life threatening to the baby. The best way to prevent serious complications is to prevent sensitization. (Learn more about the Rh factor and pregnancy on the American Council of Obstetricians and Gynecologists website.)
Group Beta Strep test: between 35 to 37 weeks
Group B streptococcus bacteria is commonly found in the gastrointestinal and genital tract. It is unrelated to strep throat. Group B strep is usually harmless in adults, but can be harmful to your baby. Possible effects including pneumonia, meningitis, and blood borne infections or sepsis. It is passed to the baby during labor.
Your provider will perform a Group B strep vaginal and rectal culture between 35-37 weeks gestation.
If you are GBS positive, you’ll be given antibiotics in labor, or after your bag of water breaks. It’s important to know your GBS status (positive or negative) when you are admitted to the hospital for labor and delivery. Read more about Group B Strep here.
Preparing for Labor & Delivery
The third trimester of pregnancy is an exciting time where you are preparing for the birth of your child. Here are a few steps you can take as you get ready to welcome the newest member of your family.
Prenatal Classes
Prenatal classes are a great way to prepare for labor and delivery, explore birthing options, and prepare to care for your newborn. Check with local providers to find classes near you.
You’ll want to time your class so that you finish it with about a month left of your pregnancy, but not more than two months. This means you’ll have time to take in the information even if your baby comes early, and will still remember the information when you need it.

36 Week Reminders
Hospital Pre-Registration
If you haven’t already done so, it’s also the time to send in your hospital pre-registration form to the hospital you’re planning to deliver at.
Group B-Streptococcus (GBS) Status
Make sure that you have been tested for Group B Strep. If you are GBS positive, you’ll need antibiotics during labor, or after your water breaks. Read more about Group B Strep here.
FMLA/Short-Term Disability Forms
If you have not already done so, discuss with your employer any forms that will need to be completed prior to your maternity leave. Please complete the forms to the best of your abilities and bring them to your next clinic visit. Once received in clinic, you can expect your forms to be completed within 4-7 business days.
For more details on Minnesota’s parental leave laws, see this pdf.
Circumcision
If you are having a baby boy and plan to circumcise, check with your insurance company regarding coverage prior to going to the hospital. Some insurance companies will not cover circumcisions in the hospital, and the cost of circumcisions is roughly double in the hospital compared to the cost in clinic after discharge.
Labor and Delivery
Labor typically begins in the weeks around your due date. Most women give birth between 37 and 42 weeks. Factors like multiples may cause you to deliver early, and women occasionally deliver after their due date as well.
Wondering when you’ll deliver? If you’ve had a baby before, this pattern may be the best predictor of when you’ll deliver this time around. If this is your first pregnancy, you may get a better idea of when you’ll deliver based on your mother’s labor and delivery history.
Am I in labor?
You are likely in labor if you experience the following symptoms:
- You are experiencing abdominal and/or back pain (i.e. contractions) every 5-7 minutes
- Each contraction lasts one minute
- The contractions persist for more than 1 hour
- You cannot talk through the contractions
Your bag of water may break before labor. Your water breaking may be a large gush of fluid or a trickle of fluid that does not stop.
Keep in mind that loss of the mucus plug (a larger, quarter size discharge of thick mucous) typically happens during the late third trimester and can precede the onset of labor anywhere from hours to weeks.

When to Call Your Provider
If you experience any of the following symptoms, don’t wait. Contact your provider immediately to ensure the best possible care for you and your baby.
- Vaginal bleeding
- Decreased fetal movement
- Preterm contractions
- Headache that doesn’t go away with Tylenol
- Significant shortness of breath or chest pain
- Sudden onset of pain, redness, and/ or swelling in the back of your lower legs
- You think you are in labor, with regular, painful contractions that are < 5 minutes apart for at least 1 hour and getting stronger and closer together over time.

Pain Relief During Labor
In general, there are two types of drugs for pain relief: 1) analgesics and 2) anesthetics. Analgesics lessen pain without loss of feeling or muscle movement. Anesthetics relieve pain by blocking most feeling, including pain. Pain relief medications can be either systemic, regional, or local. Systemic medications affect the entire body. Local medications affect only a small area of the body. Regional medications affect a lower segment of the body, an example would be from the waist down.
An epidural block (sometimes referred to as an epidural ) is the most common type of pain relief used for childbirth in the United States. In an epidural block, medication is given through a tube placed in the lower back. For labor and vaginal delivery, a combination of analgesics and anesthetics may be used. You will have some loss of feeling in the lower areas of your body, but you remain awake and alert. You should be able to bear down and push your baby through the birth canal. For a cesarean delivery, the dose of anesthetic may be increased. This causes loss of sensation in the lower half of your body. An epidural also can be used for postpartum sterilization.
Read more about medications for pain relief during labor and delivery here.
Fetal Monitoring During Labor
Fetal monitoring is used to track your baby’s heartbeat during labor. It’s normal for your baby’s heartbeat to fluctuate during labor, and especially during contractions. A normal fetal heartbeat is between 110 and 160 beats per minute during late pregnancy.
Fetal heartbeat monitoring allows your provider to determine whether these fluctuations are normal. If your baby’s heartbeat starts to exhibit abnormal fluctuation patterns, repositioning you, starting oxygen or IV fluids will be tried to resolve the problem. As a last resort, your doctor may decide it is safer to proceed with a c-section instead of a vaginal birth. Read more about fetal heart rate monitoring during labor here.
What if my baby is breech?
"Breech" means that your fetus is oriented feet or buttocks-first instead of head-first.
If your baby is breech, you may have the option of external cephalic version (ECV) to turn the fetus. Over half of ECV attempts are successful. However, if ECV is not successful or you and your baby are not in good condition for the procedure, your doctor may decide to proceed with a C-section instead of a vaginal birth. Read more about what to expect if your baby is breech here.
Labor Induction
There are situations where your health or the baby’s health requires starting labor before your body has gone into labor on its own. This is accomplished in several ways. Most commonly, hormonal medications (which are the same as the natural hormones your body makes to bring on labor) are given vaginally (Postaglandine) or through IV (Petocin). In most cases, inductions are planned well in advance giving you plenty of time to discuss the timing and procedure with your doctor. Read more about labor induction here.
Welcoming Your Baby & Postnatal Care
Congratulations, you have a new baby! What happens now? Before you bring them home from the hospital, here are a few things that will happen. Keep in mind that a regular stay after a vaginal birth is about 2 days, and a regular stay after a c-section is about 3 days. If you or your baby need a little extra care, your stay may be longer. This is common if your baby is premature and needs some extra attention in the NICU.
Before You Go Home
Right after your baby is born, they’ll usually be placed on your chest for some mom-and-baby bonding. You may have to wait to hold your baby if he or she needs immediate medical care.

Newborn Tests
Your provider will perform the following tests to make sure your newborn is healthy:
Apgar score - This test is performed at one and five minutes after birth. Your provider will test your baby’s activity, heart rate, reflexes, and breathing. This helps your provider determine if your baby needs additional medical attention.
Blood spot test - This test will check for metabolic disorders like phenylketonuria at 24 hours of age.
Hearing test - It is important to do this while in the hospital, since babies begin taking in sensory information from the world around them as soon as they’re born. Catching hearing disorders early increases the chance that treatment can help your baby make sense of the world of sounds around him or her.
*The MN Department of Health has a complete list of newborn screenings performed in Minnesota. Testing varies slightly by state. If there are other tests you’d like performed, check with your insurance and your provider before your due date to make arrangements.
Routine Newborn Procedures
- Vitamin K Shot: A newborn has incomplete liver function and lower levels of blood clotting proteins. This shot helps improve both.
- Antibiotic Eye Ointment: This is placed in the baby’s eyes but does not casue pain or irritation. It prevents eye infections for vaginal bacteria
- Hepatitis B vaccine - this can also be given at your first visit with your Hepatitis B vaccines are usually given in 3 doses: immediately after birth, around 1-2 months, and after 6 months.
- Circumcision - If you’ve decided to have your baby boy circumcised, this can be done before leaving the hospital, or as part of a follow-up visit at your Clinic circumcision is usually about half the cost of a hospital procedure. Check with your provider to see what options are available to you.
New Mother Check-Up
Before you go home, your provider will make sure your recovery is on schedule. You’ll need to be able to use (and walk to) the bathroom unassisted, keep solid food down, be free from fever or other signs of illness and your vaginal bleeding has decreased appropriately. Your doctor will also check to make sure that your uterus is shrinking normally and vaginal repairs or abnormal incisions are starting to heal.
Breastfeeding
Many new moms begin breastfeeding within the first hour of their baby’s birth, when they first hold their newborn. Don’t worry if you or your baby don’t catch on to breastfeeding right away, though - your baby may not be hungry at first, and hospitals usually have trained lactation consultants who will help you get comfortable with the process.
Why Breastfeeding?
Breastfeeding is a great way to bond with your baby and give him or her a healthy start in life. Human breast milk contains all the necessary nutrition your baby needs for the first six months, and also supplies antibodies that help protect your baby from viruses and bacteria.
Mother’s milk contains a unique and powerful combination of nutrients important for your baby’s health, growth, and development. Human breast milk is also easy for babies to digest and can promote overall health of the baby’s digestive system. Babies who are given human milk have less weight gain during their first year, and are less likely to suffer obesity than babies who are formula fed. However, breastfeeding is a personal choice, and may not be feasible for every new mother.
Postpartum Visit
Schedule a postpartum visit for 4-6 weeks after you deliver. Please call sooner if you are experiencing: depression, difficulty breastfeeding, fever, breast pain, uterine pain, increasing vaginal bleeding, significant shortness of breath, chest pain, sudden onset of pain, redness and/or swelling in the back of your lower leg.

After leaving the hospital
Self-care
Do not douche, medicate yourself for vaginal discharge, use tampons, or have intercourse for six weeks following delivery.
Postpartum Depression
Adding a baby to your home life requires significant adjustments. If you feel that you may be suffering from postpartum depression, know that you are not alone, and that there are resources available to you. Don’t wait until your postpartum checkup - contact your provider as soon as possible to get the help you need during this chaotic adjustment period.
Learn more about emotional self-care and postpartum depression here.
Postpartum Follow-Up
If you haven’t already, call your clinic shortly after going home from the hospital to schedule your postpartum check at 4-6 weeks postpartum, unless otherwise instructed by your doctor. For example, if you had a c-section, your first prenatal visit will often be sooner.
During your postpartum follow-up, your provider will evaluate your recovery and make recommendations for your care going forward.
Postnatal Care: Baby’s Physician
If you haven’t already decided on a doctor for your newborn, now is a good time to consider your options. When looking for a family practitioner, make sure your clinic offers services including:
- Well child preventive visits
- Acute childhood illness and injury
- Immunizations
- Hearing and vision screenings
- Developmental screenings
To provide the best continuum of care, consider a clinic which specializes in both prenatal care and family practice.








